
“Our unit has 100 cots and we are running at 150% capacity. You are welcome to come and work with us on sepsis, but our problem, Felicity, our problem is DATA….” Thus began my journey with Dr Simbarashe Chimhuya and Dr Gwendoline Chimhini, two neonatal consultants running Harare Central Hospital’s enormous neonatal unit, striving in the face of scarce resources, hyperinflation, industrial action and horrifically resistant Klebsiella pneumoniae. “I can’t even tell you our mortality rate by birthweight - and the records – the records are being eaten by termites! If we are to take part in research, data is where we must start.”
Fired by Dr Chimhuya's evangelical zeal, I asked colleagues at UCL whether anyone was working in this field, and was put in touch with the Neotree team, led by Dr Michelle Heys. They were developing a digital clinical decision support and data collection tool to improve care for neonates in low-resource settings. The app walks healthcare professionals through the initial assessment and resuscitation of new-borns. It provides education and diagnostic guidance along the way, while simultaneously capturing data on demographics, clinical features and planned management. Data can then be fed back on unit data dashboards, and at monthly unit meetings for quality improvement. Dr Chimhuya and Dr Chimhini were delighted with my initial demonstration of what the app could do, so now I needed to secure funding...
 |
  |
|
| Baby admitted to surgical ward at HCH (image used with maternal consent) - Copyright Charlotte Ashton | Piles of medical notes with termite damage - Copyright Dr Simbarashe Chimhuya |

We were lucky enough to receive a Small Research Grant from the Healthcare Infection Society, who provided £10,000 in funding to pilot the implementation of Neotree at Harare Central Hospital and see what the impact of a new script (NeoLab) was in reducing time to receive blood culture results from a daunting median of six days (Chimhini et al, IPIP). I had a moment of panic when we were awarded the grant. We were essentially going to implement a prototype electronic medical record system in a hospital without reliable power, let alone WiFi, in the space of 12 months with £10,000.
I should have had more faith in my Zimbabwean colleagues. From the first time I talked one of the junior doctors through the admission and discharge script, hovering anxiously to see if she had any questions, she looked at me in a bemused way and politely said she could take it from there. The next morning, I asked the night doctor if he’d managed to use the app at all (hoping against hope he’d managed at least one admission): “Oh yes, I did all thirteen”.

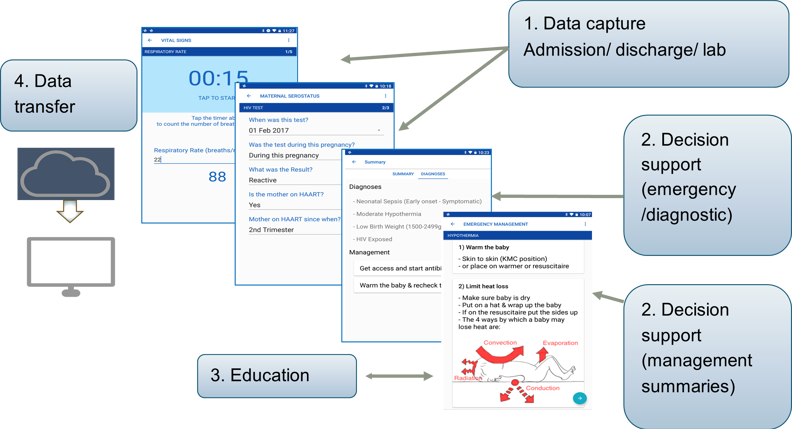
Nearly three years on, currently funded by a Wellcome Digital Innovation grant, Neotree is now running in three hospitals in Zimbabwe and Malawi. We have captured data on more than 13000 babies, trained over 350 healthcare workers and demonstrated sustained improvements in antimicrobial prescription rates (Gannon et al. BMJ Open Quality), hypothermia and even in nursing rota cover (papers in draft). Neotree aims to be a Learning Healthcare System combining data capture, decision support, education and continuous learning with the end goal of improving patient outcomes. For example, Neotree data, linked with blood culture results, are being used to develop a clinical diagnostic algorithm for neonatal sepsis, alongside other decision support algorithms (Neal et al. in draft). We are working closely with the Zimbabwean Ministry of Health Electronic Medical Records team to ensure Neotree can be integrated into nationwide plans for the digitalisation of medical records; and in Malawi to ensure integration with the District Health Information Software 2 (DHIS2). Our next step is an (as yet unfunded) stepped wedge trial across twelve hospitals in two countries to analyse the impact of Neotree on neonatal mortality. Best of all, Neotree data are being used by Zimbabwean and Malawian healthcare professionals in their own quality improvement projects, in areas such as congenital syphilis and late preterm outcomes.
 What humbles me most about Neotree is the utter commitment and passion of our Zimbabwean and Malawian colleagues for the project. They have carried and grown Neotree, despite the pressures, challenges and fear of the COVID-19 outbreak, including for the past 18 months without any UK project staff on the ground in Zimbabwe or Malawi. Due to their sustained hard work, flexibility and innovation, we have been able to demonstrate the impact of the COVID-19 pandemic on the neonatal units in which we work (Chimhuya et al, MedRxiv), and rapidly fed back data on stillbirth rates to hospital executives and Ministries. Underpinning their commitment is the appreciation of the power of data - although there is much to do, data are the first step. In Dr Chimhuya’s words: “Before Neotree we were working in the dark. Now, we have switched on the light - at least we can see the room in which we are working.”
What humbles me most about Neotree is the utter commitment and passion of our Zimbabwean and Malawian colleagues for the project. They have carried and grown Neotree, despite the pressures, challenges and fear of the COVID-19 outbreak, including for the past 18 months without any UK project staff on the ground in Zimbabwe or Malawi. Due to their sustained hard work, flexibility and innovation, we have been able to demonstrate the impact of the COVID-19 pandemic on the neonatal units in which we work (Chimhuya et al, MedRxiv), and rapidly fed back data on stillbirth rates to hospital executives and Ministries. Underpinning their commitment is the appreciation of the power of data - although there is much to do, data are the first step. In Dr Chimhuya’s words: “Before Neotree we were working in the dark. Now, we have switched on the light - at least we can see the room in which we are working.”
 For more information on how to support Neotree, or work with them, please visit neotree.org
For more information on how to support Neotree, or work with them, please visit neotree.org
Could HIS support your next research project? Find out more about our funding and awards.